大腸直腸癌 即時照護網
| 訊息: |
|
|
分期及預後
AJCC 8TH 更新:多了"IVC"分期及對區域淋巴結更明確定義
| 參考資料 | 根據美國癌症協會 American Joint Committee on Cancer (AJCC) 8th 版翻譯 | 2017/8/24 |
|---|---|---|
| 分期 | 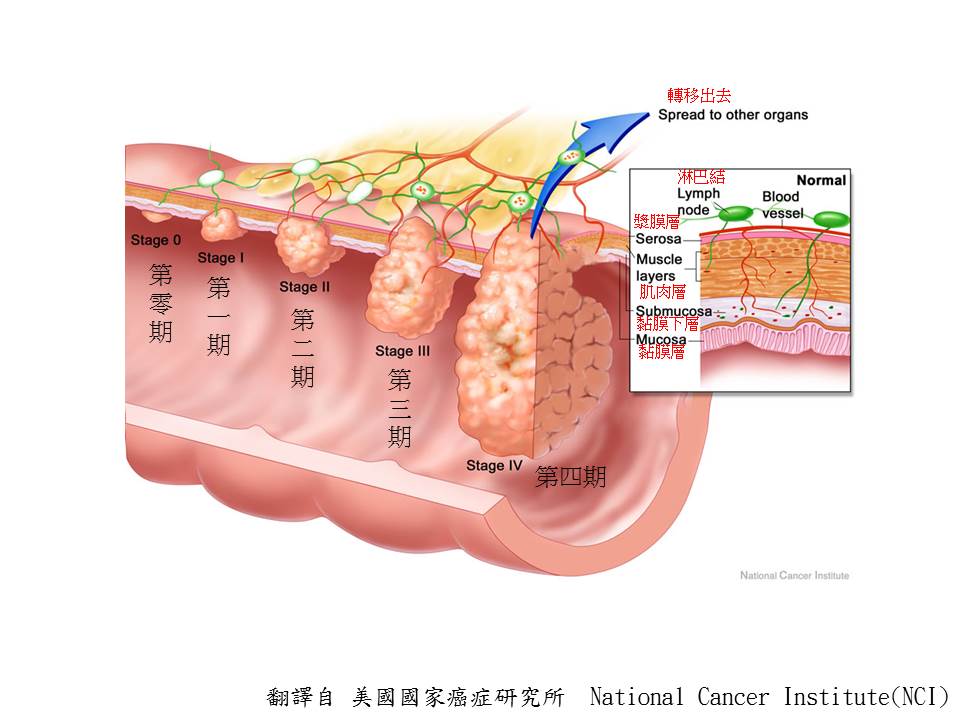 |
2017/8/24 |
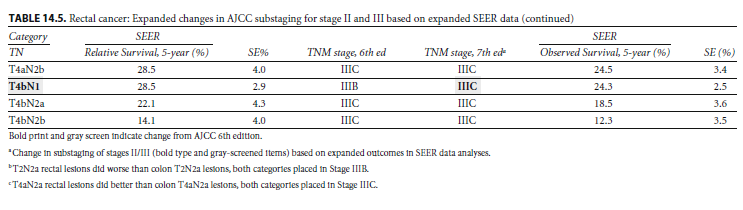
| 第一期 | 腫瘤侵犯到黏膜下層或肌肉層,沒有局部淋巴結之轉移,沒有遠處轉移。 | |
| I | 腫瘤侵犯到黏膜下層(T1) | |
| I | 腫瘤侵犯到肌肉層(T2) | |
| 第二期 | 腫瘤穿過肌肉層至漿膜層或無腹膜覆蓋之大腸及直腸周圍組織,沒有局部淋巴結之轉移,沒有遠處轉移 | |
| IIA | 腫瘤穿過肌肉層至大腸及直腸周圍組織(T3) | |
| IIB | 腫瘤穿過肌肉層,大腸及直腸周圍組織並穿透漿膜層至大腸及直腸周圍組織(T4a) | |
| IIC | 腫瘤穿過肌肉層,大腸及直腸周圍組織並穿透漿膜層,大腸及直腸周圍組織至周邊組織或器官(T4b) | |
| 第三期 | 區域淋巴轉移 (N1a=1;N1b=2-3;N2a=4-6;N2b>=7),沒有遠處轉移 | |
| IIIA | T1–T2 N1/N1 c | |
| T1 N2a | ||
| IIIB | T3–T4a N1/N1c | |
| T2–T3 N2a M0 | ||
| T1–T2 N2b | ||
| IIIC | T4a N2a | |
| T3–T4a N2b | ||
| T4b N1–N2 | ||
| 第四期 | 遠端轉移 | |
| IVA | (M1a)轉移侷限在一個器官/位置(例如,肝,肺,卵巢,非區域淋巴轉移) | |
| IVB | (M1b)轉移超過一個器官/位置 | |
| IVC | (M1c) 轉移侵犯腹膜 | |
| 區域淋巴結 | Cecum: Pericolic, ileocolic, right colic; Ascending colon: Pericolic, ileocolic, right colic, right branch of the middle colic; Hepatic nexure: Pericolic, ileocolic, right colic, middle colic; Transverse colon: Pericolic, middle colic;< Splenic flexure: Pericolic, middle colic, left col ic; Descending colon Pericolic, left colic, sigmoid, inferiol l1lesentenc; Sigmoid colon: Pericolic, sigl1loid, superior rectal (hemorrhoidal), inferior mesenteric Rectosigmoid: Pericolic, sigmoid, superior rectal(hel1lorrhoidal), inferior mesenteric Rectum: Mesorectal, slIperior rectal (hemoIThoidal),inferior mesenteric, internal iliac, inferior rectal (hcmorrhoidal) |
|
| 更多資訊 | Peritoneal lavage cytology in patients with curative resection for stage II and III colorectal cancer:
A multi‐institutional prospective study Results A total of 1378 patients were eligible for analysis. The number of patients with pStage II‐III colorectal cancer was 670 and 708, respectively. Fifty‐four patients (3.9%) had positive cytological results. In pStage II patients, the 5‐year RFS rates with positive and negative cytology were 61.1% and 81.6%, respectively (p = 0.023). The 5‐year OS rates were 67.1% and 91.7%, respectively (p = 0.0083). However, there was no difference in RFS or OS between pStage III patients with positive and negative cytology results. The peritoneal recurrence rates were 11.8% and 1.5% in pStage II patients with positive and negative cytology results, respectively (p = 0.032). These rates were 10.5% and 2.5% in patients with stage III disease, respectively (p = 0.022). Conclusion Stage II colorectal cancer patients with negative cytology had better outcomes than those with positive cytology. Peritoneal lavage cytology is useful for predicting peritoneal recurrence after curative resection of stage II‐III colorectal cancer. 暫時無法影響期別判定(AJCC VIII 無定義),但是高風險。 |
Ann Gastroenterol Surg. 2024 May 27;8(5):807 AJCC VIII |
| 更多資訊 | The ITBCC group recommends the use of a three-tier system as used by Japanese Society for Cancer of the Colon andRectum: 0–4 buds—low budding (Bd 1). 5–9 buds—intermediate budding (Bd 2). 10 or more buds—high budding (Bd 3). per 0.785 mm2 This system allows for risk stratification of both pT1 colorectal cancer and stage II colorectal cancer. In pT1 colorectal cancer, Bd 2 and Bd 3 are associated with an increased risk of lymph node metastasis whereas in stage II colorectal cancer, Bd 3 is associated with an increased risk of recurrence and mortality. The ITBCC group recommends that, in addition to the Bd category, the absolute bud count is provided (eg, Bd 3 (count 17)). This avoids loss of information that may occur when applying a cut-off to borderline cases. For example, a bud count of 9 (Bd 2) may be biologically similar to a bud count of 10 (Bd 3), but falls into a different risk category. |
ITBCC) 2016 Mod Pathol . 2017 Sep;30(9):1299 |
簡單來說,存活資料有三種定義:
(1). Overall Survival: 不管任何死因,死亡就是登記為死亡(event 事件),"總體的存活率"。
(2). cancer-specific Overall Survival: 如果我們能夠知道死亡的原因,死亡原因跟癌症相關,這種死亡才算事件(event),那這個叫做"癌症專有存活率"。
(3). relative Overall Survival: 在大規模的臨床資料,很難知道詳細的死亡原因,這時候會根據"沒有"癌症病人的死亡率,用年紀,性別,種族..等因子做校正,就
可以大略推估出所謂"相對的"死亡率,(接近於癌症專有存活率)
可以大略推估出所謂"相對的"死亡率,(接近於癌症專有存活率)
| 預後圖 | 注意: 存活由長到短排列大約是 I > A(II/III) > B(II/III) > C(II/III) > IVA > IVB ,換言之, 第二期不一定活得比第三期長) | 2014/11/5 |
|---|---|---|
| 大腸癌 | 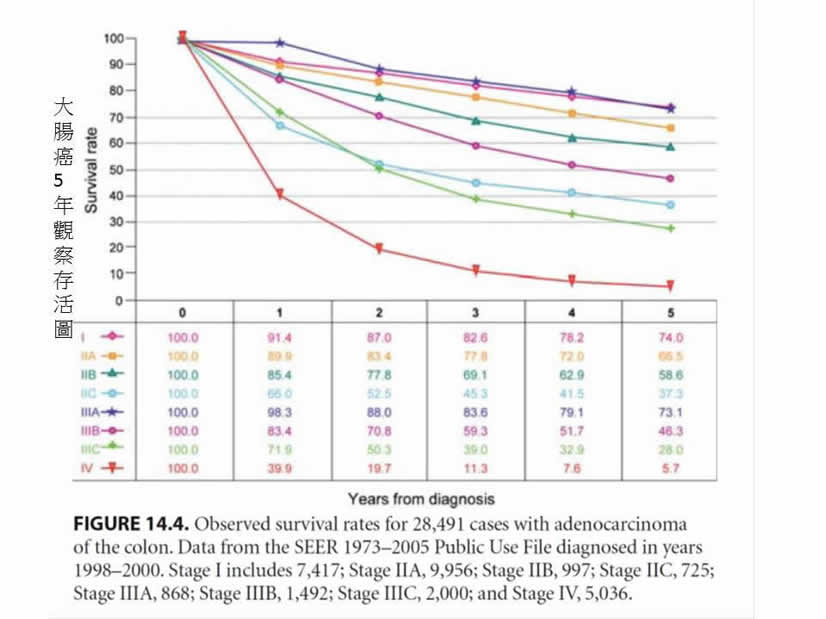 |
|
| 直腸癌 | 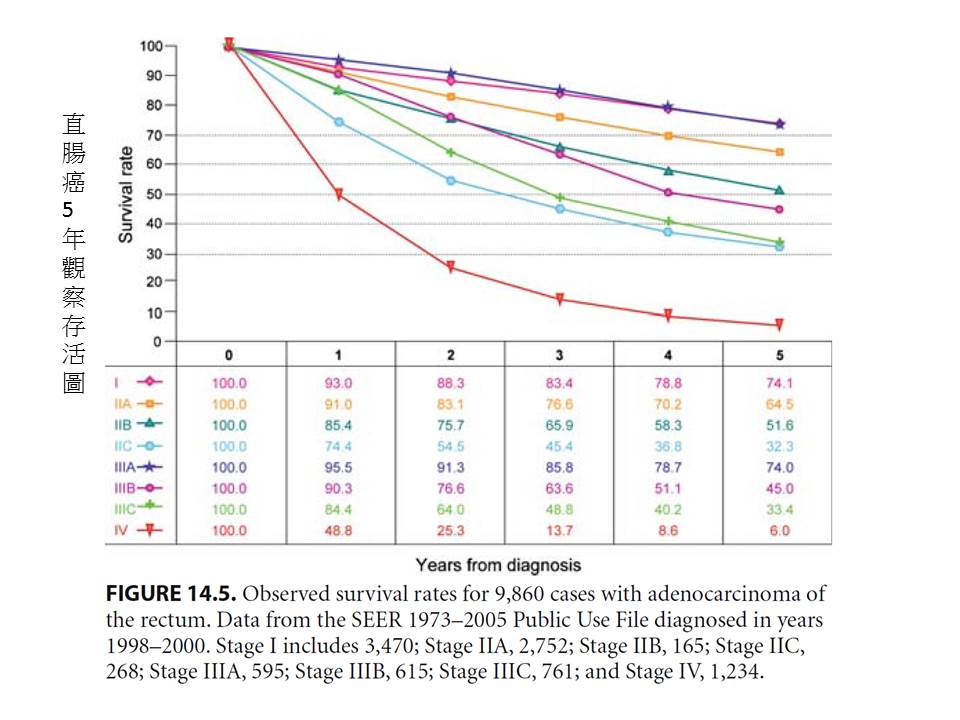 |
|
| 直腸癌 復發率 | 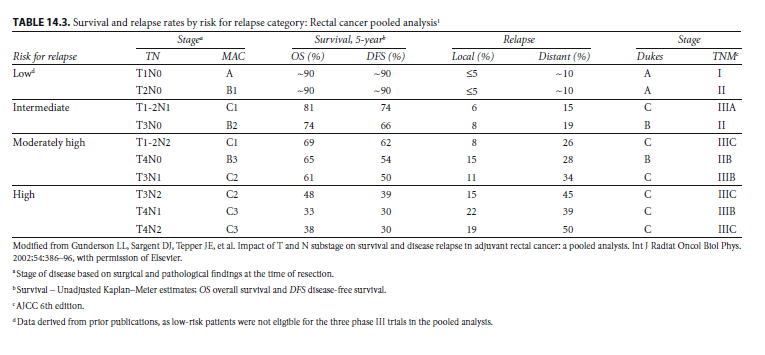 |
|
| 大腸癌 | 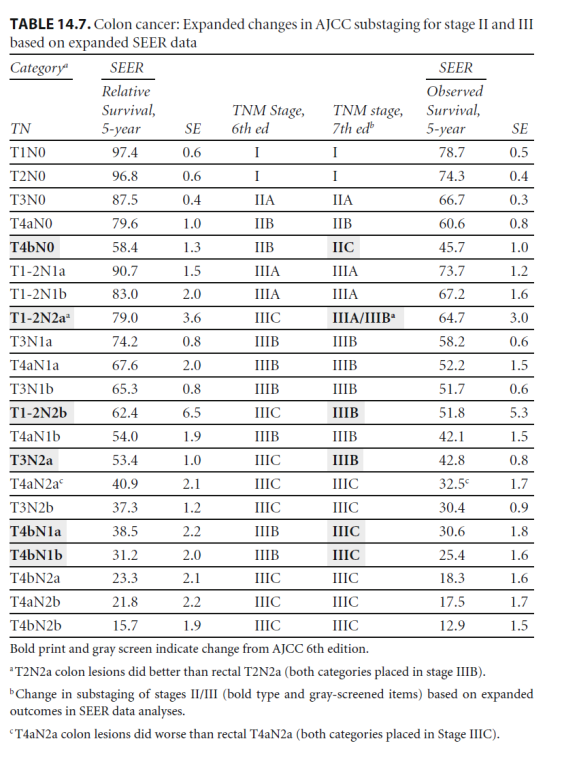 |
|
| 直腸癌 |
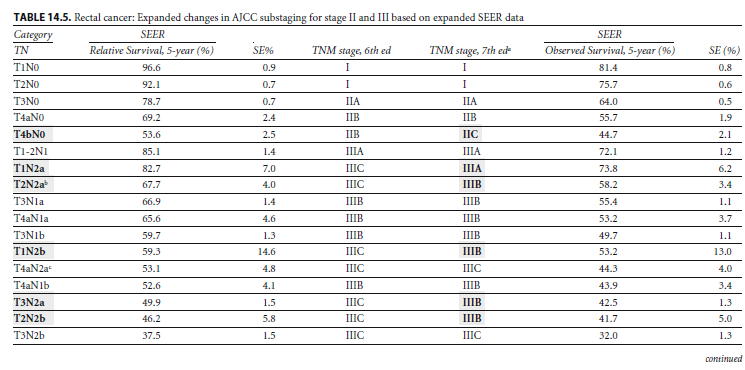
5年大腸癌 "相對"存活表(細項): 指死於癌症 |
|
|
5年直腸癌 "相對"存活表(細項): 指死於癌症 |